First, I am not "pro" weight loss drugs, nor am I "anti" weight loss drugs. I agree with Michael and Aubrey that some of the discourse around semaglutide is problematic and that fat phobia is rampant, awful, and something that we need to work to abolish. Nothing in this article or anything else I produce is intended to undermine the fundamental truth that fatness in no way determines or reflects a human being’s value, or to imply that fatness is an individual failing. The sole purpose is to accurately communicate scientific knowledge about a topic that is highly charged and often misinterpreted in popular media.
Science communication as a field is extremely difficult, and miscommunications arise due to both the way scientists present information and also the way journalists or media personalities interpret it. Science is extremely nuanced, but I firmly believe that laypeople are more than capable of understanding said nuances and details without the science needing to be overstated or oversimplified. Both of these issues are common and problematic; in fact, a lot of “fake news” could be described as "oversimplifying" or "overstating."
Many of the errors in this podcast might seem like “semantics” or unimportant, but a pattern of consistent errors and misunderstanding data is problematic. Despite their best efforts, this episode contains a lot of knowledge gaps and unfortunately is a good example of why subject matter expertise is important when attempting to evaluate sources and communicate about science. Unfortunately, many of their chosen sources were from mainstream media outlets, which only serves to amplify the media’s already poor science communication.
A question I’m grappling with is “what standards do we want to hold journalists to?”. This episode contains mistakes that are verifiable via a Google search, and don’t require expert knowledge. I, personally, would like to live in a world where career journalists are researching and sharing information in a responsible manner and seeking out expert review when discussing topics they are not knowledgeable about.
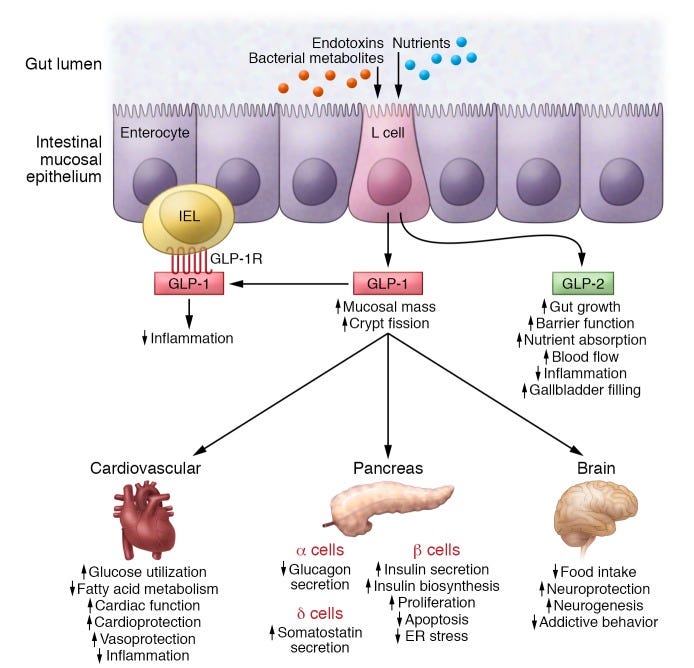
For those who are interested, I thought it would be useful to do a quick overview of how semaglutide works. Contrary to what Aubrey and Michael state in this episode that scientists don’t really know how GLP-1 RAs work, we actually DO know how they work. Semaglutide (and other GLP-1 RAs) bind to GLP-1 receptors and effectively replicate the effect of GLP-1. While the primary action of GLP-1 is to stimulate insulin secretion, it also plays a role in glycemic control, inhibition of gastric motility, suppression of glucagon secretion, and the stimulation of satiety (see figure below from the scientists who discovered GLP-1). GLP-1 RAs do the same things! I will provide some additional links at the end of the article that cover this in more depth.
A quick note that I am aware there is a “part 2” to this but it is only on Patreon, so I wasn’t able to access it. Ok, on to the episode:
His name is Dr. Daniel Drucker, and he discovers a new hormone in humans, which is GLP-1. It's called glucagon-like peptide 1.
For some historical context, Daniel Drucker did not discover GLP-1, despite US-centric media outlets reporting this. There were three scientists who were working on GLP-1 in parallel: Daniel Drucker, Joel Habener, and Jens Holst. This work began in the 1970s and Drucker was a research fellow in Habener's lab in the 1980s. This is why all three scientists were awarded the Canada Gairdner Award in 2021. It's also worth highlighting here that Svetlana Mojsov was an essential piece of the puzzle and has not been appropriately credited.
And [Dr. Drucker] discovers that those Gila monsters have genes for something called exendin-4, which, when sort of synthesized in a lab eventually became Ozempic.
John Eng was the first to isolate exendin-4 from Gila monster venom in the 1990s at the VA in New York, not Daniel Drucker.
Researchers don't totally know the mechanism for what makes GLP-1 agonists work the way that they do.
Scientists definitely do know how GLP-1 receptor agonists work (see explanation of semaglutide mechanism of action above, as well).
And so, it works by you end up eating less because you just basically feel full after each meal. So, it triggers your satiety hormone.
It’s a common misconception that there is a single "satiety hormone." In true “bodies are complex and cool” fashion, there are many hormones that regulate satiety. Michael might be aware that many hormones contribute to satiety and is merely attempting to simplify information, but my concern is that such oversimplifications perpetuate "pop science" and open the door to people developing an incorrect understanding of how the body works.
There are stories that are told about the initial presenting of the research on these at the American Diabetes Association Conference and people were weeping and gave it a standing ovation… Because what they're talking about is people whose A1c’s went from like 11 to 7. From really heightened urgent risk down to a pretty safe range just with this one drug.
I’m not sure where they found these numbers. The average baseline HbA1c level in the STEP 2 trial was 8.1%, and patients with HbA1c levels over 10% were excluded: there weren’t people with HbA1c levels of 11 in this trial. The mean reduction in HbA1c levels after 68 weeks was 1.6% in the 2.4 mg group and 1.5% in the 1mg group. The standard error for the mean % change was only 0.1, which suggests that the vast majority of people were pretty close to that mean difference. It is also worth noting that there doesn't appear to be great evidence to inform what a clinically meaningful decrease in HbA1c is. While I have seen several publications reference 0.5% per NICE and ADA guidelines, I cannot find the underlying research. If anyone can find that, please let me know!
Diabetic version hovers at around $900 a month. And it costs more for weight loss, it costs like one $1300 a month out of pocket, and most insurers do not cover it.
$900 for Ozempic is without insurance. Multiple state Medicaid plans cover Wegovy and, as of April 2022, they had 80% commercial formulary access. Additionally, Novo Nordisk told CNN in November that 80% of insured patients in the US taking Wegovy are paying less than $25 a month. Here is an interesting article about the cost of weight-loss drugs in the US and elsewhere: How do prices of drugs for weight loss in the U.S. compare to peer nations’ prices? - Peterson-KFF Health System Tracker. I know that without context this seems like an absurdly expensive drug (and yes, it definitely is expensive), but if you look at drugs for other chronic conditions, it’s actually on the lower end. For example, Pfizer and Eli Lilly both have newly FDA-approved drugs for inflammatory bowel disease (IBD) which have list prices of about $6,000 and $10,000 per month, respectively. And those prices are par for the course for IBD drugs! At the end of this fact check, I do discuss the issues with the cost of these drugs, but it has much more impact on a payer-level (i.e., insurance companies and health plans) than the individual level.
When a drug goes on the FDA's shortage list, the FDA then allows what are called compounding pharmacies to mix up what is basically their own version of that drug without prior FDA approval or screening.
The issue with this statement is in the phrasing “the FDA then allows…”. It is true that there are fewer restrictions on compounding drugs that are on the shortage list and qualify for an exemption under section 503B of the FD&C Act, but this is not synonymous with approval. The FDA did not ever issue support for compounding pharmacies to be making compounded semaglutide; the compounding pharmacies took advantage of a policy that exists to provide medically necessary drugs during shortages to get in on the $$. If this feels overly nitpicky I understand, but to me this is just another example of how beneficial an expert review would be for the podcast: it might even open up the potential for an episode about the FDA.
it's not Ozempic and it's not Wegovy. It might be a watered-down dose of those things. It could be something called semaglutide sodium.
Just to clarify, Ozempic and Wegovy are both semaglutide, just different dosages. Importantly, Wegovy and Ozempic are the base form of semaglutide base. These compounding pharmacies are largely unable to obtain semaglutide in its base form, and are instead obtaining semaglutide-salt. This isn’t a “watered-down” dose of semaglutide, but an entirely different drug. This is why it is problematic. As Jasmine Gonzalvo, a professor in the College of Pharmacy at Purdue University in Indiana said, “These differences in solubility could affect the rate and extent of absorption of the compounded formulations, particularly when combined with other ingredients.”
Well, except this is not roughly the same thing and is hazardous to human health. Semaglutide sodium is not cleared for use in humans because it is bad for humans.
There are no studies examining the safety of semaglutide sodium, so it is incorrect to say “it is not cleared for use in humans because it is bad for humans”. Compounded semaglutide was harmful in many instances, but that is not the same as establishing that semaglutide sodium is bad for human health. Lack of safety studies does not automatically equal something being harmful.
It's like there's a shortage of this drug, so we're just going to let people buy it from weird, fly-by-night, carnival barker ass companies selling whatever the fuck on the internet, we're not going to regulate it at all?
The FDA does not endorse compounding pharmacies and is very explicit about being cautious because products from compounding pharmacies are not FDA-approved. This would have been a good opportunity to look into the FDA regulation of compounding pharmacies, including Section 503A and 503B. It is a bit dense but it’s interesting. This letter from the New Jersey Attorney General provides a good overview, too!
There's not an enforcement mechanism beyond these letters so far. Like, they're not doing more than that yet, at least not in reporting.
There is no enforcement mechanism because what the compounding pharmacies are doing is a legal loophole; this is definitely something that needs to be addressed, but it’s wrong to imply that the FDA has the ability to do more but is choosing not to.
As we're talking about these compounding pharmacies, big weight loss companies are buying up these startups. WeightWatchers bought one of these and their stock price jumped almost 60% in a day.
WW did not buy a compounding pharmacy. They bought an online weight management platform. I’m not shilling for WW or saying it’s a good thing, but they bought a startup where medical professionals would be working with clients. It’s in no way a compounding pharmacy.
They are funded by Novo Nordisk, of course.
Hopefully this is a statement of the obvious and not an implication that this is bad, given that Novo Nordisk is the one that is making the drug, and this is how the pharmaceutical industry works. Here is a great (very short) article from the former CEO of Eli Lilly about the nuance of “sponsoring” a trial. It makes total sense that a drug company is the one to finance its own clinical trials. If you think about it, why would any organization volunteer to shell out millions of dollars to test a drug that they have no stake in?
So, step one is like the overall, just like, "We're going to give fat people semaglutide for weight loss." Step two is the same thing, but on people with type 2 diabetes. Step three is semaglutide with intensive behavioral therapy.
STEP 1 is testing semaglutide vs placebo among people "with overweight or obesity" WITHOUT diabetes, not just "fat people". This is an important distinction, because the objective of the study is to see how people WITHOUT diabetes respond. Studies had already established that semaglutide induced weight loss in adults with T2DM (the SUSTAIN trial). STEP 2 is testing semaglutide vs placebo in people with Type 2 diabetes and "overweight or obesity" but it also tested safety and tolerability by comparing two different doses of semaglutide. So, not the same as STEP 1 "but on people with type 2 diabetes" as Michael said. STEP 3 tested semaglutide vs. placebo with intensive behavioral therapy. Here is a great article summarizing the STEP trials 1 through 5: Semaglutide 2.4 mg for the Treatment of Obesity: Key Elements of the STEP Trials 1 to 5 - Kushner - 2020 - Obesity - Wiley Online Library
…step six and step seven are focusing on East Asian folks. It's worth mentioning that most of these trials, for Wegovy in particular, are just overwhelmingly white, as many diet studies are. One of the sort of leading meta-analyses of studies involving over 11,000 participants was 80% white, 10% black, and 5% AAPI.
Unfortunately, all clinical trials have a race problem, it's not just diet studies. This is very well-established, and the National Institute on Minority Health and Health Disparities works specifically on this issue! I’m not sure which meta-analysis he’s referring to, but it would be great if Michael provided more citations in general.
Step 6 and Step 7 were conducted separately in East Asian populations because the definition of obesity is different in those populations (Korean Society for the Study of Obesity, Japan Society for the Study of Obesity). Studies have shown that East Asians tend to have higher percentages of body fat compared to non-Asians with the same BMI (Deurenberg 2002, Jee 2006). People of East Asian descent also tend to develop some conditions that are obesity-related at a lower BMI compared to non-Asian individuals (Kodama 2013, Shai 2006, Huxley 2008). As a result, the BMI cut off for obesity in East Asians is ≥25, compared to ≥30 for non-Asians. It is important to note here that BMI is an imperfect measure of adiposity and we have previously discussed that it is not independently a good measure of health status. For this reason, both the Korean and Japanese guidelines include the measurement of visceral fat via weight circumference, in addition to BMI, when evaluating cardiometabolic risk.
So, roughly 80% of people who take semaglutide lose some amount of weight, roughly 5% of their body weight. And roughly half of people who take semaglutide lose 10 to 15% of their body weight.
Per the summary of the STEP trials that Michael and Aubrey linked to on the episode page, 86-89% of patients lost >=5% of their body weight. That's more than 80% but also, that's only counting those who lost >=5% of their body weight which is not the same as losing "some amount of weight." This is an incorrect interpretation of the data. An even greater proportion of participants lost “some amount of weight”, but the statistic that Aubrey reported is specific to >= 5%. Additionally, far more than 50% lost >=10% (69-74% based on that same review). They later also state that “we're talking about a drug that 50% of people who take it will lose 15% of their body weight,” which again doesn’t accurately reflect the results.
So, like a one in two chance of losing like a moderate amount of weight.
This is not an appropriate statement to make: aside from the fact that more than 1 in 2 patients lost a substantial percent of their body weight, you cannot extrapolate population averages to the individual outcomes. This exact issue is one of the pitfalls of BMI - it may be predictive on an aggregate level, but it doesn't necessarily indicate risk at an individual level. Michael is also failing to account for the comparison group here. It's not just how much weight the treatment group lost, it's also how much they lost compared to the placebo group.
So, for about a third of patients, they're losing maybe three times as much weight as previous interventions.
I’m not sure where this statistic came from, if you can find it, please send me a link!
The side effects of the drugs seem to be almost universal. Some studies find-- I think the lowest one I found was like 60% of people have gastrointestinal symptoms, but then some of them are finding like 93% of people. So, it's like nausea, constipation, diarrhea, vomiting, the sort of tummy stuff that you would associate with pretty significantly fucking with your hunger and satiety hormones.
There is a very important distinction to be made between "symptoms". This is why adverse events (AEs) are graded based on severity. In the STEP trials, specifically, AEs were classified as “mild (easily tolerated, causing minimal discomfort and not interfering with everyday activities), moderate (causes sufficient discomfort and interferes with normal everyday activities) or severe (prevents normal everyday activities)” (See the STEP 1 Supplementary Appendix for more information). While certainly some people have very bad side effects, the rates of serious adverse events were quite low and, tellingly, the percent of patients who discontinued semaglutide due to side effects was under 7% in all the STEP studies (notably, it was 12% for liraglutide in STEP 8). Patients taking placebo also discontinued due to adverse events. This is why the comparison to placebo is important.
There's been some worry about pancreatitis. Some trials find that it increases, but then there's a trial of liraglutide that finds that it actually decreases.
Current evidence suggests no association between semaglutide and pancreatitis: "When combining all phase 3a data, pancreatitis occurred in five semaglutide-treated patients in PIONEER (six in the comparator group), and in 15 patients in SUSTAIN (13 in the comparator group)." Of course, because it is such a rare outcome, we cannot rule out any risk. That's what post-marketing studies are for! I can't find the trial Michael mentions here that supposedly finds that liraglutide is associated with decreased risk of pancreatitis (though I can find several studies to the contrary).
And there's a study out of China last year that shows that this mechanism exists in mice where it basically stops bowel function.
Also can't find this, I really wish they’d include a list of all of their sources.
Yeah. And you know two people dying is nothing to--
This is a bit scary, both because it’s a fundamental misunderstanding of how this industry works and it’s also getting a little too close to the anti-vax arguments ("I know someone who died after getting the vaccine!"). Earlier in the episode, they acknowledged the AE database is not reliable (Michael said, “But we don't sort of know what to make of those things because the Adverse Events database, as we've discussed on the show before, it's like anyone can submit cases, so it's basically just like a hotline.”). We don't actually know whether those deaths were due to semaglutide. But even so, many approved medications have scary side effects, but people still take them because it's a probability of a bad thing vs the certainty of a worse thing (i.e., the indication you are taking the drug for).
What you find in most of the studies is almost everybody is getting some side effect or another, and they typically happen in the first couple of weeks of the study when you're upping your dose. It actually takes four months to get up to the 2.4 mg, like weight loss dose, but it typically goes away as people kind of get used to the drugs. And so, in the two-year study, there were 150 people who completed the two-year trial, and only 10 of them dropped out due to adverse effects, which is only 6%. So, what this indicates is that people are getting side effects, but most, like the vast majority of people are willing to push through the side effects and complete these trials.
This is how SO many drugs work: antidepressants and birth control are examples that many people are familiar with.
So, what you're saying is folks are more likely to stay in these studies than other studies into sort of like how folks can lose weight.
I’d love to look at this but don’t know what exact studies they’re referring to.
The first is that the populations that are being studied in these trials are actually relatively narrow… They're also excluding people with a lifetime history of a suicide attempt, any history of myocardial infarction, stroke, hospitalization, any kind of existing cardiovascular stuff, known or suspected abuse of alcohol or recreational drugs, and female who is pregnant, breastfeeding, intends to become pregnant or is of childbearing age, and not using a highly effective contraceptive method.
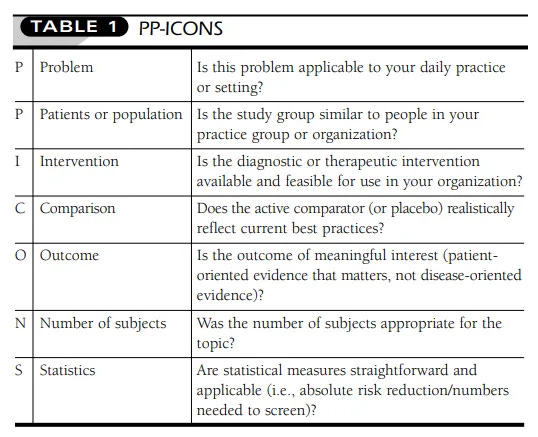
This is true of almost all clinical trials, it’s not unusual or something that undermines the trial results. It does, however, impact external validity (i.e., who can we generalize these results to?). It is clear from this episode that Aubrey and Michael lack expertise and knowledge to assess clinical trials. I’ll take this opportunity to delve into that a bit here - but feel free to read on if you aren’t interested! Consider, for example, that you have invented a pillow that you believe leads to better sleep for the average adult than a standard pillow. Now you want to do a study to see if it works the way you believe it will. Would you choose to include someone taking sleep medications? Probably not, because that would interfere with their assessment of the pillow. Would you include someone with a newborn baby who they have to attend to multiple times a night? Probably not, because, again, that would interfere with their assessment of the pillow. This is a very basic example, but I’m trying to frame it in a less scientific way. The other piece of this, which Aubrey and Michael neglect to mention, is that there are very intense laws around including pregnant people in clinical trials. This is a good thing! We do not want to expose a fetus to an experimental therapy. In general, there are a few important things to look at when you are evaluating a clinical trial. My favorite tool for non-scientists is called PP-ICONS (I cannot vouch for the name but at least it’s memorable). It was developed by Dr. Mark Flaherty as a tool for clinicians, but I think it is really helpful for everyone. PP-ICONS stands for: Problem, Patient or population, Intervention, Comparison, Outcome, Number of subjects, and Statistics. The table below shows how to evaluate each component of PP-ICONS. I recommend reading the paper that the table comes from because it provides a great example of using the PP-ICONS tool. I welcome suggestions from readers of other tools and strategies for assessing clinical trials, as well!
You can already see, as we're sort of like walking through this research, the gap between the popular claims that are being made about these drugs and what the research actually says.
This is first and foremost a media issue, not a science issue. With respect to real-world findings, though, this is a common phenomenon known as the “efficacy-effectiveness gap.” And it is not specific or unique to weight-loss drugs. There was actually a great 2017 study that found that the efficacy-effectiveness gap for GLP-1 RAs and DPP-4 therapies in T2D was largely explained by non-adherence among real-world patients.
And basically, it's like people start regaining the weight very quickly. And within a year, they've regained almost all of the weight. These drugs seem to put people in the same cycle as fad diets, but just with more dramatic and longer results.
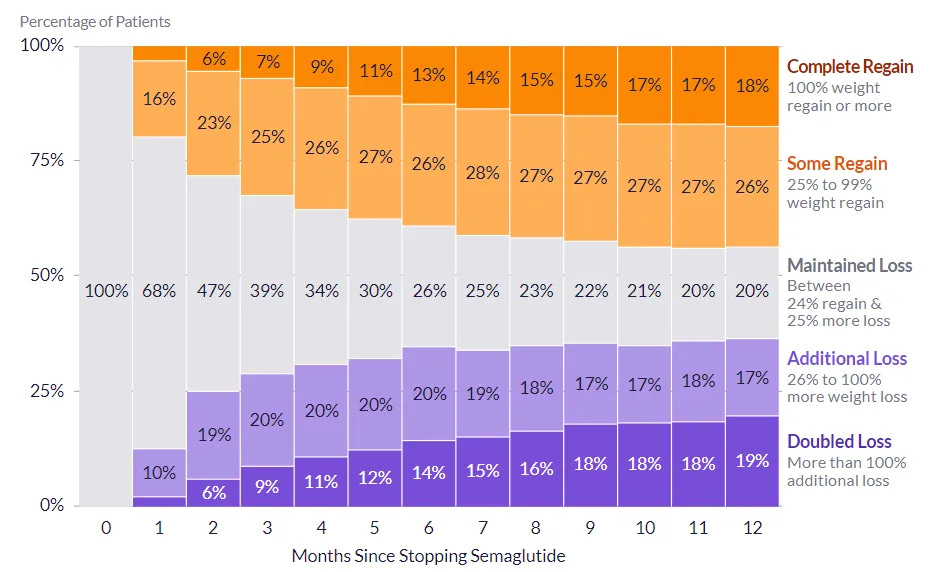
There are many medications which people need to take for a lifetime; the same is true for antidepressants or any drug for a chronic condition. We know that fatness isn’t a choice or due to a lack of willpower any more than high blood pressure is, so yes managing a chronic issue requires long term interventions. These drugs aren't putting anyone in a "cycle" unless they are not taking them under appropriate guidance and comparing them to fad diets is highly problematic. Interestingly, Epic, the electronic health records giant, recently did an analysis of over 20,000 patients who discontinued semaglutide or liraglutide and they found that “the majority (56.2%) of patients either remained around the same weight they were at when stopping the medication or continued to lose additional weight” (see graph below for semaglutide results). Of course, this is not peer-reviewed (not that peer-review necessarily makes data legitimate - but that’s a whole other post), but it is an interesting report, nonetheless! This analysis doesn’t investigate the clinical and demographic characteristics associated with regain vs maintained or additional loss, but I contacted the authors and they replied that they would look into it in the future!
And that is people's plan for how this is going to happen, and that's not how these drugs work.
Whose plan?
I'm seeing this discourse among weight loss clinicians too, where they're like, "Well ultimately it comes down to diet and exercise and so we need to get people on these drugs and then teach them the diet and exercise stuff. And then once they know that, we can take them off the drugs."
This might be a case of miscommunication between science and media: the media might be portraying it that way, but medical professionals and scientists are not. The conclusion section of the Step 5 study says, “these results support the benefit of continued semaglutide treatment for sustained weight loss.” Here are some examples of online articles/videos intended for lay-audiences that feature medical professionals explaining that these drugs are intended to be for chronic use:
"Well, Ozempic does work if you can stay on it." Okay, but people aren't staying on it. We know from real world data that even when it's fucking free, people are not staying on it.
Real-world adherence to almost every medication is terrible, especially for chronic conditions. A frequently cited statistic comes from an admittedly old 2003 report from the WHO which cites some even older papers and says that “in developed countries, adherence among patients suffering chronic diseases averages only 50%.” I think this statistic keeps being used because it is easier than summarizing all the new literature. But there is recent literature that supports this! A recent systematic literature review found that 20% of patients with multiple sclerosis do not adhere to their medication, and 25% discontinue their medication before 1 year. A study from 2008 looked at seven chronic health conditions and found that, “72.3% of individuals with hypertension achieved adherence rates of 80% or better compared with 68.4%, 65.4%, 60.8%, 54.6%, 51.2%, or 36.8% for those with hypothyroidism, type 2 diabetes, seizure disorders, hypercholesterolemia, osteoporosis, or gout, respectively.” These are just a few examples - there is a substantial body of literature looking at non-adherence, including the economic and morbidity/mortality consequences. Anyway, the point is that this is not unique to semaglutide!
As part of this campaign, Novo Nordisk has specifically courted black public figures and particularly black women as spokespeople.
I couldn’t find any sources saying that they specifically courted black public figures to represent this campaign. If they did, I'm not sure how that's really that problematic. That's how marketing works - you find spokespeople who represent the demographic you are marketing to. That's not a Novo Nordisk thing, it's a capitalism thing.
Very few people are asking fat people what they need in this moment. And nobody is asking diabetic people what they need in this moment.
Genuinely wondering what this would look like. KFF did actually do a survey and found that 59% of Americans trying to lose weight would be interested in taking a safe and effective weight loss drug. Most importantly, though, that number dropped to 14% when they were told they might gain weight back after stopping use. That seems to me like asking fat people what they want! And the answer is mostly that they don’t want a drug they have to take forever.
Concluding thoughts
Some actual concerns about semaglutide
Despite the promising health benefits of semaglutide, there are some very real reasons for concern. In my mind, there are two big issues that we, as a society, need to address with respect to this class of drugs. First, is just the sheer amount of money that our healthcare system (note: not individuals, but the system as a whole) might be paying for these drugs. Medicare is currently prohibited by law from covering weight loss drugs, however, the Treat and Reduce Obesity Act of 2023, which is currently in the House, would reverse this and allow Medicare drug plans to cover weight loss drugs. An article in NEJM from March 2023 calculated that if even 10% of Medicare beneficiaries who are obese (per CDC prevalence estimates) began taking brand-name semaglutide (Wegovy), we’d be looking at an additional $26.80 billion in annual Medicare spending. For reference, this is ~18% of the total Part D spending in 2019. While some of this cost may be offset by decreased future costs (due to improvements in cardiometabolic health, for example), it would obviously be an immense upfront cost. In fact, some insurers have already stopped covering Wegovy due to the ballooning costs (see this article about the North Carolina State Health plan and this article about University of Texas employee healthcare plan. It’s worth noting that this isn’t an entirely new phenomenon - in 2014, there was a similar crisis about potential Medicare spending for hepatitis C drugs. What ended up happening, actually, is that the prices dropped substantially as competitors popped up. It is likely the same thing will happen here, but we are in a bind until then.
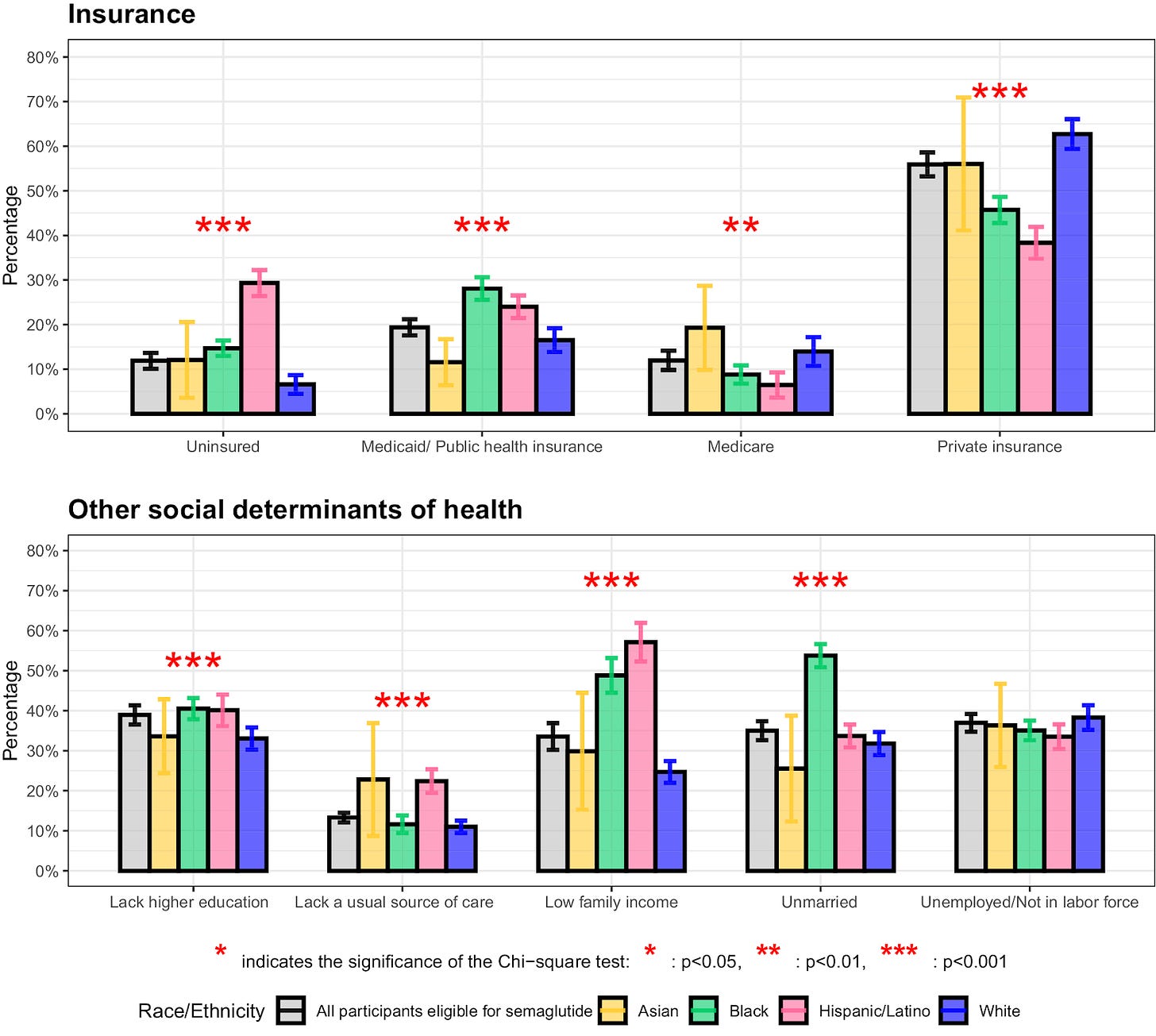
A second really important issue when it comes to these new weight loss drugs is the matter of equity. The health disparities that exist in the US today are unacceptable. Long standing structural inequities and systemic racism have resulted in a paradigm in which the racial and ethnic minorities experience a significantly greater burden of disease compared to White people (note that there are, of course, significant health disparities in other groups, as well, but I’m focusing on race/ethnicity here because it is the most salient with respect to weight loss drugs). A recent study used NHANES data to examine financial barriers to semaglutide access among adults eligible for semaglutide treatment (for either weight loss or diabetes) and found that, compared with White individuals, a significantly higher percent of Black and Hispanic individuals were uninsured, lacked a usual source of care, had low family income, or lacked higher education (see below for Figure 2 from the paper, “Racial and ethnic differences in financial barriers and social determinants of health among semaglutide‐eligible adults, 2015 to 2020”). The evidence on the actual disparities here are lacking, though. This is consistent with an Epic Research report that CNN covered which found that more than 70% of semaglutide prescriptions have gone to White patients and a Komodo analysis which reported that 65% of prescriptions for Ozempic, Mounjaro, Wegovy, and Rybelsus went to non-Hispanic White people. Obviously, we have a lot of work to do to address healthcare inequities in this country, and this is just one example.
Finally, there has been quite a lot of media frenzy about the muscle loss with semaglutide. It's a frequently cited statistic that 40% of the weight loss in the STEP 1 trial was fat-free mass (i.e., mass composed of muscle, water, organ, and bones). While this is true, it ignores the fact more than 50% of the weight lost in the placebo arm was fat-free mass (1.17kg fat mass and 1.48kg lean body mass). This is why we have placebo arms in trials - to provide context for the treatment effects. It is important that we consider the loss in the semaglutide arm with the loss in the placebo. Most notably, semaglutide resulted in a net increase in the proportion of lean body mass relative to total body mass by 3.6%. These data are all available in the supplementary appendix for STEP 1.
New and interesting research since the episode was released
Since MP put out the Ozempic episode, there have been several “real-world” studies (this just means they are observational) of semaglutide published. These studies have been conducted in a variety of countries, which is pretty interesting! The SURE (SemaglUtide Real-World Evidence) program is a joint effort of 10 countries (Canada, Denmark, France, Germany, Italy, the Netherlands, Spain, Sweden, Switzerland, and the UK) to conduct 9 observational studies investigating once-weekly semaglutide in patients with T2D in routine clinical practice. All 9 studies found that patients with T2D taking semaglutide had clinically meaningful reductions in HbA1c and body weight. These findings were replicated by a study in Saudi Arabia, a study in Macedonia
Two other recent studies with interesting results:
First, a real-world study of over 100,000 individuals with overweight or obesity (scientific definitions, not my choice of wording) taking “anti-obesity” drugs and found that, compared to non-GLP-1 RA “anti-obesity” medications, semaglutide was associated with lower risk of suicidal ideation.
Second, a real-world study of over 1 million drug-naive (i.e., untreated) individuals with T2D which found that, compared to other drugs for T2D (metformin, insulin, SGLT2 inhibitors, sulfonylureas, and thiazolidinediones) GLP-1RAs were associated with decreased risk for colorectal cancer. The maximum follow-up for the study was 15 years, though the average follow-up was not reported which makes it harder to critically evaluate the findings. I do think it is still an interesting analysis, though!
More MOA links




Holy heck! Your stuff is so good, thank you for doing all this analysis!
As a non-science guy, I think I fundamentally agree with Michael and Aubrey's project and their message, that the media, the weightloss- and wellness industry, and even the medical field, are unfortunately very anti-fat.
That being said, I've often found weird inconsistencies listening to Maintenance Phase. Like in the "Is Being Fat Bad For You" episode, they criticise that there is much more attention on the direct health effects of obesity than the negative health effects of anti-fat bias. Which is true, and it is a massive media issue, but then they get into the studies, and it almost sounds like they criticise the studies for how the media portray their findings, which is kind of nuts.
But I would never have caught or have a reason to suspect that stuff like the gallbladder cancer thing is wrong, that's a wild oversight to me. I also fully believed Aubrey saying that there are no evidence-based methods of weight-loss, and only now realise that they've never fully explained what that means.
The wildest thing to me is in the "Forks Over Knives" episode about vegans and vegetarians. They talk about Forks Over Knives, essentially a propaganda film that promotes veganism by wildly exaggerating the beneficial health effects of a vegan diet.
Michael and Aubrey repeatedly point out that they think that veganism and vegetarianism are good, but that the film is harmful because it overstates its claims and spreads misinformation.
And, like, that's exactly what Maintenance Phase is doing with regards to anti-fat bias. It's a real issue that deserves to be talked about, but there is no need to disparage all studies into obesity or adipose tissue. Dieting can definitely be harmful, and it doesn't have to cause cancer for that to be true.
You mention media criticisms a couple of times in your posts here, and I think it's best to view Maintenance Phase primarily as media criticism. It's a real issue when Michael and Aubrey do not draw a clear line between media criticism and science communication, and essentially do their own science communication without (as far as I know) any background in science.
Anyway, great job!
An amazing piece, as always.
1. I like your initial criticism on journalism, though I do think it is quite calm. We need to be held accountable more for the mistakes, the poor research we are conducting and for the lack of expertise in some areas. It is sad, because very specialized journalists in niche topics are slowly disappearing, especially as a result of media closures. Try to find a Romanian journalist that understands semaglutides - maybe there is 1 or two.
2. I cannot wait for the Maintenance Phase to respond to this newsletter series. They better accept their mistakes and seek guidance on how to research better. If they go the opposite route, then they are a bunch of fools.
3. A lot of misinformation around the drug.
3.1. What I am worried about is whether or not this will prompt changes in our diet culture or will continue the same but having a drug as a backup to cover for "the bad food". The equity aspect is important, because not everyone has access to it.
Just some thoughts.